Is refractive eye surgery for you?
Ophthalmologists have come a long way in the past 20 years since they began reshaping corneas for improving vision. Initially this was performed by actually cutting slices into the cornea by hand, like spokes on a wheel, in a procedure known as radial keratotomy (RK). Now much more highly sophisticated technical equipment is used, such as lasers, making the procedures easier on both patient and eye doctor, as well as safer and more precise. Before all pilots who are getting good vision by relying on harmless pieces of curved glass start lining up for these procedures, they should put these surgeries into perspective, both from the point of view of their general visual health as well as their FAA medical certificates.
Briefly, the concept of refractive surgery involves changing the shape of the interface of the cornea and the outside air. If you remember your high school physics, you will recall that light bends when it travels from one density to another. This is what happens when you look at your feet while standing in a swimming pool…your legs look bent. When light traveling through air meets the curved surface of the cornea (water density), the shape of the cornea determines where in the back or your eyeball it will focus, relative to the length of your eyeball. In people with perfect vision, that point occurs on a small spot on the retina, and minor adjustments are made by the lens to fine-tune that focus for the differences in distances of the object being viewed. Most of us have corneas that are not perfectly shaped. Some corneas are too flat, resulting in far-sightedness (hyperopia) while others are too pointy, causing near-sightedness (myopia). Others are curved irregularly, causing a condition called astigmatism. It should be noted that the age-related problem of close-up vision difficulties (called presbyopia) has nothing to do with the shape of the cornea, as it is the lens that becomes less pliable over time. This condition therefore is not treatable by refractive surgery, unless one considers having one eye corrected for near vision and the other for distant vision. More on that later.
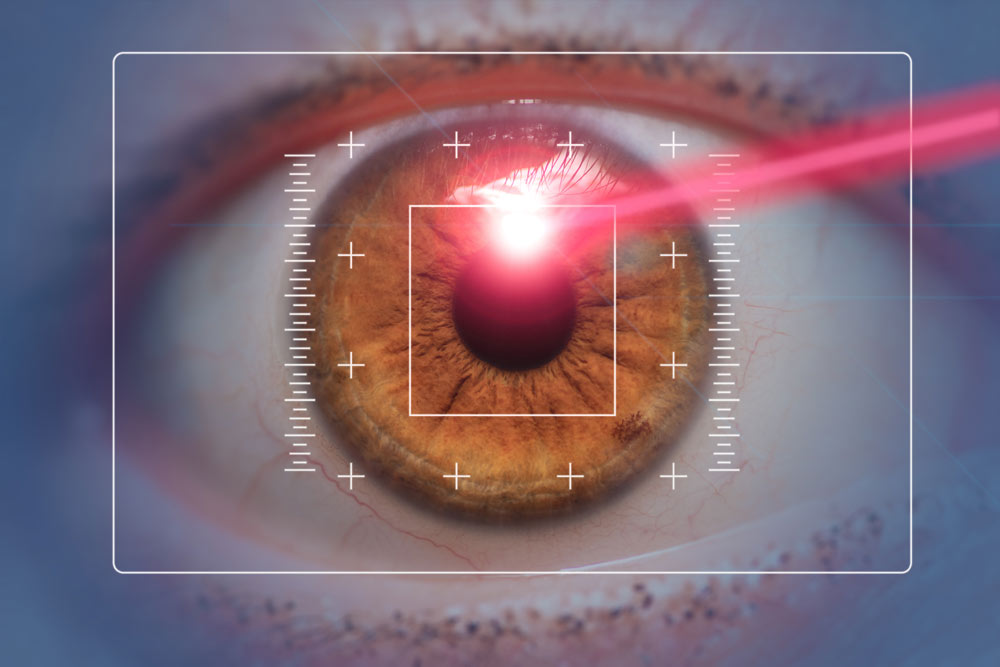
Nowadays, the 2 most commonly offered surgeries are photorefractive keratectomy (PRK) and laser assisted in situ keratomileusis (LASIK). The former involves literally vaporizing the outermost layer of corneal cells with a laser, the latter involves slicing a thin flap (but still attached by a hinge piece) off the central cornea and then reshaping the layer of cornea underneath with a laser. When the desired shape is obtained, the flap is placed back onto the cornea and allowed to heal in place. PRK is done less than LASIK these days, as the latter is the newer technique and offers a number of advantages over the older procedure. For example, the “recovery time”(which means time one can see well enough to go back to work in a regular job, not necessarily to return to flying…will go over that later) can be as short as 2-3 days…in fact some eye doctors feel comfortable enough to do both eyes at the same time.
It must be pointed out that as in any surgical procedure, complications can happen to anyone, and for a pilot, even some of the more minor complications can interfere with qualifying for a medical certificate.
Occasionally potential vision-threatening complications occur, such as infection, development of haze in the vision, scarring, night glare, perforation of the eye, and prolonged post-operative steroid drop use which can result in cataracts or glaucoma. Less devastating but problematic complications of LASIK include detachment or movement of the flap resulting in double vision, growth of corneal tissue into the flap, bleeding into the white part of the eye, and technical problems associated with the instruments. Also somewhat common, but usually temporary, are problems with mild irritation, dryness, sensitivity to bright lights, and tearing.
In order to have the best results from LASIK, certain selection criteria should be kept in mind. First and foremost is the health of the patient and their eyes. People with corneal diseases, collagen vascular diseases, pregnancy, or side effects from steroid medications should not undergo these procedures. Patients should be older than 18 years of age, and should have “stable” refractive errors to begin with. Without giving you the
meaningless formula, this means people who can be expected to have good result with refractive surgery, not individuals whose corneas are so severely misshapen that they cannot obtain reasonable results. Pupil size must be small enough that when in the dark, the edge of the pupil does not expand beyond the edge of the corneal flap, resulting in a condition where night glare would occur. Most importantly, the patient should have realistic expectations. Although these techniques have become extremely precise these past few years, no one should undergo these procedures with the expectation that they will obtain perfect vision. Some folks can only get improvement, and may still need to rely on glasses for perfection. It is also important to reiterate that the loss of clear close-up vision that comes with age cannot be altered by surgery, and that such patients undergoing this procedure may still need to wear reading glasses.
After surgery, one should not rub the eyes, and contact sports should be avoided at least 6 months, as it might dislodge the healing flap. For the pilot it is also important to know the FAA requirements to maintain their medical certification.
To date, because of the slight increased risk that a hard blow to the head could cause the post operative cornea to rupture, military pilots are not allowed to have refractive surgery done, either before or during their flying career. Corneal mapping is generally done on military applicant pilots to exclude those that have had these procedures, although the military is currently researching the feasibility of changing that rule. Most airlines do not have any such limitations as long as the pilot meets acceptable FAA standards. Let me now walk you through those standards for civilian airman, both private and commercial, because the guidelines are the same, and a waiver is no longer required.
The FAA’s requirements are based on 2 principles, the first being that the eye surgeon verifies complete healing has taken place and that vision has fully stabilized. For LASIK, visual stabilization usually occurs within 3 months, and residual night glare can be expected to diminish within 6 months. In some people, this can occur much more rapidly. The ophthalmologist needs to fill out an FAA form called “Report of Eye Evaluation” Form 8500-7, which must be submitted to the FAA. This can be done directly or through your AME. Secondly, as in any other situation, your vision must meet the standards for the class of medical certification requested, whether with or without corrective lenses. That part has not changed.
There is one interesting new opportunity worth mentioning for those of us who wear bifocals. Near the beginning of this article it was stated that corneal surgery is not useful to correct presbyopia, which is the situation where near vision is adversely affected due to the aging of the lens. For this common condition, some ophthalmologists are recommending surgery to correct one eye for near vision and the other for distant vision, rendering the person essentially monocular. In other words, one would use one eye to visualize objects far away, and the other for close vision. This same effect can be achieved with contact lenses, a situation which the FAA does not allow because it destroys depth perception. Despite this fact, the FAA does now allow this surgical procedure to be done on pilots. The reasoning is that, in contrast to contact lenses which are removed regularly, the surgery makes this a continuous and permanent condition and thereby allows the person to eventually learn depth perception by experience, just as an individual who physically loses one eye learns depth perception by integrating other visual clues. The FAA requires the pilot who has this done to use glasses or contacts that correct both eyes for near and distant vision while flying for six month period afterward, in order to allow time for this adjustment to occur. Thereafter, the pilot may apply for a Statement of Demonstrated Ability (SODA) and undergo a medical flight test with an FAA examiner in order to get the corrective lenses restriction removed from his or her medical certificate.
Now, with all the above information, is refractive surgery right for you? There are a variety of individual questions that must be answered, and they are all different for each and every pilot. Consideration should be given to the fact that most insurance companies do not cover this procedure, and can cost up to $2,500 per eye. Also, one must think about the sick-leave from work. In a non-flying job, this may be less of a problem, unless complications are encountered. In a flying-related job, consideration must be made that it make take several months for vision to stabilize enough for FAA approval. I frequently advise airline pilots to refrain from refractive surgery until they retire, as complications may permanently interfere with their careers. Unless the use of glasses or contacts presents a severe annoyance in the cockpit, or uncorrected vision is so terrible that suddenly being without one’s corrective lenses might produce a safety hazard, this surgery can be considered cosmetic and might best be done when one’s livelihood no longer depends on passing the FAA medical examination.
One final point…whether pilot or not, one should never be talked into this kind of surgery by an aggressive eye doctor. If you really are interested in this, carefully choose your ophthalmologist. Find out who performs the most procedures, has done them for the longest time, and who has had the best results in your community. Speak with former patients, and never hesitate to get second opinions from other ophthalmologists.
